Prostate Cancer
Digital Rectal Examination
The digital rectal examination (DRE) is the placing of a finger in the rectum to palpate the prostate by your family doctor or urologist. This gives us an indication of risk of prostate cancer. It is not diagnostic but if it is hard or irregular it raises the possibility of cancer . A normal DRE does not exclude malignancy.
A normal DRE does not exclude malignancy.
Prostate Specific Antigen
Prostate Specific Antigen is released from the prostate and enters the bloodstream. This can be measured by a blood test which has now been available in Australia for 25 years. A lot of controversy surrounds PSA testing due to its accuracy. It is a very useful test and gives us a lot of information but it cannot be diagnostic of Prostate cancer. Although it is specific for the prostate it is not specific for prostate cancer. It can increase with BPH and with infection. It is also possible to have prostate cancer with a very low PSA as not all prostate cancer makes PSA and some of the more aggressive ones may not.
The most commonly asked question is “What is a normal PSA?”. There is no answer to this question as normal implies “no cancer” to most people. There is an age related reference range and if your PSA is above this you have a greater than 25 % chance of malignancy, but if you are below it you can still have a cancer. The rate of change of your PSA is a very important factor. Change of more than 0.75 in consecutive years can be significant. You may also have a Free to total ratio checked and this gives your urologist additional information about your risk. The lower the ratio the higher the risk of cancer.
Although this test has its limitations it is still very useful when interpreted properly by your urologist.
Multiparametric MRI
Recently there have been great advances in imaging of the prostate particularly with MRI scanning. Unfortunately at this stage this is not medicare rebatable. It is also very important that the MRI is done at a radiology practice with experience in doing and interpreting this test. Your urologist will determine if you need an MRI based on your DRE and PSA. MRI cannot replace the need for a biopsy but it helps isolate the potential abnormal area in the prostate and the local extent of the disease which may be important in planning your treatment.
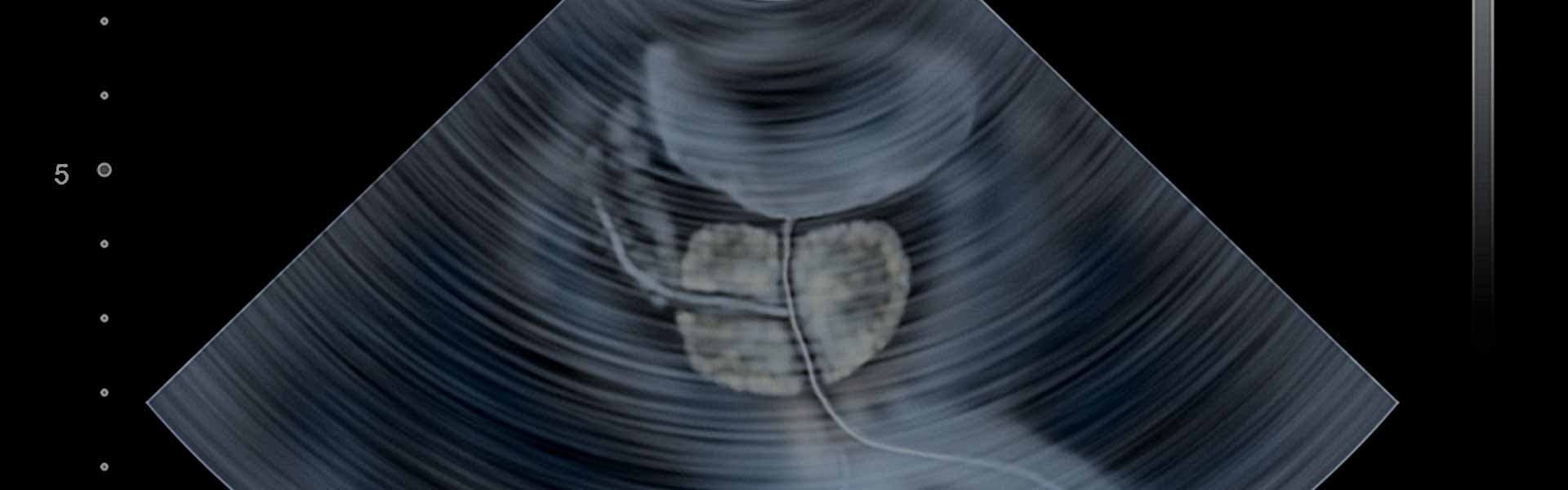
Prostate Biopsy
There are 2 different techniques used for prostate biopsy. It can be done either transrectal or transperineal. Your urologist will explain the difference and which one is available to you at a particular hospital. Dr Gassner performs biopsies using both methods.
The biopsy will give us tissue for a pathologist to make the definite diagnosis of whether or not there is cancer.
The biopsy will not only detect cancer but will give us a good indication of how widespread the cancer is within the prostate and the grade of the cancer. The grade is the Gleason score.
Gleason Score
This is the recognised system used to grade prostate cancer. Prostate cancer can be low, intermediate or high grade and this will determine the treatment options. Although the Gleason score is out of 10, it is very rarely below 6. It is made up of 2 numbers and reported as the total, ie 3+3=6, 3+4=7, 4+4=8 etc. A score of 6 is low grade, 7 is intermediate and 8 or higher is high grade.
Bone Scan and CT Scan
Once you have a positive diagnosis of prostate cancer you may be sent for these investigations to determine whether or not the cancer has macroscopically spread out of the prostate. These tests can’t exclude microscopic spread. The bone scan is a nuclear medicine study that looks for spread to the bones and the CT scan looks for spread to lymph nodes.
Treatment of Localised Prostate Cancer
The treatment of prostate cancer is a decision making process between the patient and the urologist based on patient factors and cancer factors. There is no single treatment that can be labelled the best treatment. The best treatment is the one that suits the patient and their cancer. Surgery and Radiotherapy are considered treatment options with curative intent and Active Surveillance is now also considered an option for appropriate patients.
The best treatment is the one that suits the patient and their cancer.
Active Surveillance
This is considered in patients with low volume, low grade disease that is not palpable to avoid over treating a cancer that may never cause a problem. It is still a form of active treatment with curative intent and requires regular testing with repeat PSA, DRE, MRI and biopsies. If the disease parameters change the patient can progress to surgery or radiotherapy.
Surgery
Surgery is considered for localised Prostate cancer as the aim of surgery is to cure the disease. More recently however it is also being considered for low volume nodal metastatic disease to get good local control of the disease.
Radical Prostatectomy is the complete removal of the prostate gland with some surrounding tissue and the seminal vesicles. It can be done either by open surgery or by Robot assisted laparoscopic surgery. Dr Gassner performs both methods and will discuss these with you. With both methods the repair is done over a catheter and this will usually stay in for 5- 8 days. If you have the procedure done by open surgery you may still be in hospital on day 5 post surgery and have your catheter out before you leave but with Robotic surgery you will usually recover quicker and be discharged after 2 or 3 days so you will still have the catheter in and Dr Gassner will arrange its removal.
The main advantage of Robotic Surgery is the quicker recovery including quicker return to work and less post op analgesia requirements. There is also some anecdotal evidence that return of continence is quicker.
Both methods may have the side effects of affecting erectile function and continence. If appropriate a bilateral nerve sparing procedure can be performed which improves the chance of regaining erectile function post operatively. The chance of regaining your erections is very dependent on your preoperative erectile function. To improve the continence you will be instructed on how to do pelvic floor exercises prior to the surgery and will be offered to see a physiotherapist who specialises in this area. You have a very good chance of regaining your continence but it may take 6-12 months.
Radiotherapy
The aim of radiation therapy is also curative and can be given as external beam or by using implants known as Brachytherapy. Dr Gassner has a close association with Radiation Oncologists in all 3 areas where he works and will arrange an appointment for an opinion if necessary.
Radiation therapy can also be used after surgery for cases where the disease may be quite extensive and there is a higher risk of local recurrence.
Watchful Waiting
In the elderly or patients who are medically not fit for curative therapy we will sometimes recommend that treatment is not immediately necessary. This is because prostate cancer generally grows slowly and if the cancer does cause problems or spreads it can be treated with hormonal therapy which can control but not cure the disease for some years.
Advanced Prostate Cancer
Once cancer is advanced and has spread out of the prostate we will almost always adopt a team approach and this will be discussed at a MultiDisciplinary Team Meeting with Radiation and Medical Oncologists to determine the best treatment. This will usually be a combination of Hormone therapy and Chemotherapy and may involve Radiation therapy to particular sites of spread.